Bones are living tissues made of collagen fibres filled with water and mineral salts like calcium phosphate that give them rigidity and strength. Even when they have reached adult shapes and sizes, they constantly renew and remodel by resorbing old bone and rebuilding it anew. However, after 30 years of age, females lose 8% of bone mass every ten years.
206 bones that make up our skeleton are not just giving us support, shape, protection and movement, they also produce and store bone marrow. Despite our bones being five times stronger than a steel bar of the same weight, without proper care, it can lead to brittle bone disease, osteoporosis.
For better bone health, there are 5 things we need to know about them.
1. Calcium
Calcium has a primary role in building and maintaining bone. In adults, the total body calcium content is about 1kg, 99% of them reside in the skeleton. Most people need to eat plenty of good sources of calcium for healthy bones throughout life, especially for adolescents and adults over age 50 (see box 1).
The main sources of dietary calcium are dairy milk, cheese (not soft) and yoghurt (see box 2). On average, about 35% of calcium is absorbed from the diet. Patients who cannot achieve an adequate calcium intake through the diet may need additional supplementation. In general, calcium supplements >500mg are poorly absorbed, so doses higher than this should be given as divided doses. Calcium is also better absorbed with meals. However, some foods reduce calcium absorption, such as phytates (present in cereals, bran and soybeans) and oxalates (present in spinach, walnuts and rhubarb).
Calcium supplements are usually well tolerated. The most common side effects are gastrointestinal upset, constipation, bloating and flatulence.

2. Vitamin D
Vitamin D has an important role in maintaining bones by promoting the absorption of calcium. Although some vitamin D is found in the diet (e.g. fatty fish and fortified milk) the primary source is from exposure to sunlight because dietary sources commonly provide less than 100IU (international unit) daily and are insufficient to protect against vitamin D deficiency.
The current recommended daily intake of vitamin D for preventing deficiency is 200IU for people aged 0-50, 400IU for people aged 51-70 or people with dark skins, and 600IU for people aged over 70. For patients with, or at risk of, osteoporosis the recommended daily intake is 800-1000IU.
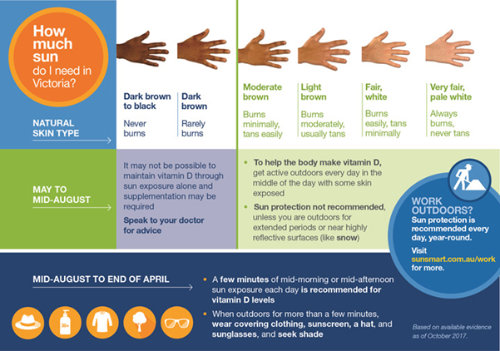
In Australia, the current recommended exposure of sunlight required to produce adequate vitamin D is approximately 15% of the body (i.e. hands, face and arms) for 5-8 minutes daily in summer and 20-30 minutes in winter, 4-6 times per week. Before 10 am and after 2 pm (standard time) for moderately fair-skinned people, which should produce about 1000IU of vitamin D daily. However, darker-skinned ethnic groups require greater daily sunlight exposure (see box 3).
3. Exercise
Regular exercise stimulates the production of new bone tissue. High-impact exercises such as aerobics, jogging, or racquet sports are beneficial; weight-bearing exercise including gentle yoga or tai chi helps to strengthen areas where the bone is stressed.
Australian guidelines recommend weight-bearing, muscle strengthening and low-impact exercises for patients with osteoporosis. Resistance training (3-5 times a week) or regular walking (90-280 minutes a week) has shown to increase bone mineral density (BMD).

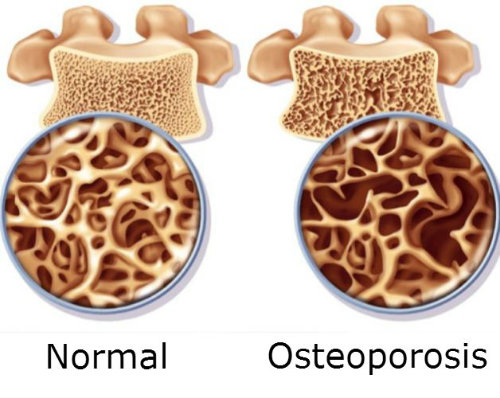
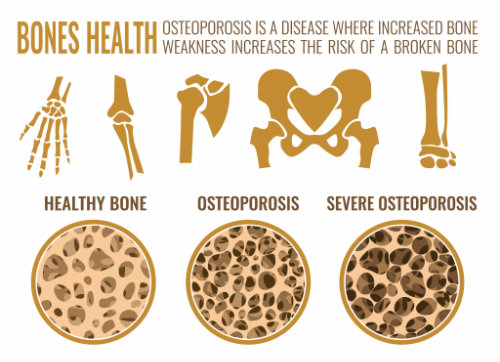
4. Osteoporosis
Osteoporosis is a ‘silent disease’. This condition remains without symptoms until a fracture occurs. In 2013 there was one osteoporotic fracture every 3.6 minutes in Australia and by 2022 there will be one osteoporotic fracture every 2.9 minutes.
It occurs due to deterioration of the bone structure, loss of bone mass and changes in bone metabolism when we don’t eat enough calcium-rich foods or if we don’t top up our vitamin D through diet or sun. It can also result from hormone changes in later life. It has become a major public health burden, it happens to one in every two women, and one in three men, over 60 will have a fracture in their remaining lifetime. There are some good online fracture risk calculators to predict future fracture risk, such as
‘Risk calculator’ by Garvan Institute in Sydney
https://www.garvan.org.au/bone-fracture-risk/fracture-risk-calculator
WHO Fracture Risk Assessment Tool (FRAX)
5. Screening and lifestyle
At present, bone mineral density (BMD) measurement is the most convenient and accurate estimate of bone strength. Other than this, a healthy lifestyle minimises the risk of developing osteoporosis and prevent further bone loss and reduce the risk of secondary fractures.
Below are important lifestyle choices for all postmenopausal women and older men
- Adequate but safe exposure to sunlight as a source of vitamin D
- Maintenance of a healthy weight and BMI
- Cessation of smoking
- Avoidance of excessive alcohol consumption.
- Identifying falls risk
- Balanced diet
Box 1: The recommended dietary intake of calcium is different for people of different ages and life stages.
Age and life stage | Recommended dietary intake of calcium (mg/day) |
Babies 0–6 months – breastfed | approx. 210 mg |
Babies 0–6 months – formula-fed | approx. 350 mg |
Babies 7–12 months | 270 mg |
Children 1–3 years | 500 mg |
Children 4–8 years | 700 mg |
Children 9–11 years | 1,000 mg |
Adolescents 12–18 years (including pregnant and breastfeeding young women) | 1,300 mg |
Women 19–50 (including pregnant and breastfeeding women) | 1,000 mg |
Women 51–70 | 1,300 mg |
Men 19–70 | 1,000 mg |
Adults over 70 | 1,300 mg |
Box 2: Good dietary sources of calcium include:
Food type | Examples | Calcium per serve (mg) |
Milk and milk products | Milk, yoghurt, cheese and buttermilk | One cup of milk, a 200 g tub of yoghurt or 200 ml of calcium-fortified soymilk provides around 300 mg calcium. Calcium-fortified milk can provide larger amounts of calcium in a smaller volume of milk – ranging from 280 mg to 400 mg per 200 ml milk. |
Leafy green vegetables | Broccoli, collards (cabbage family), bok choy, Chinese cabbage and spinach | One cup of cooked spinach contains 100 mg, although only five per cent of this may be absorbed. This is due to the high concentration of oxalate, a compound found in spinach that reduces calcium absorption. By contrast, one cup of cooked broccoli contains about 45 mg of calcium, but the absorption from broccoli is much higher at around 50–60 per cent. |
Soy and tofu | Tofu (depending on the type) or tempeh and calcium fortified soy drinks | One cup or 260 g of tofu contains around 832 mg of calcium. One cup of tempeh contains around 868 g of calcium. 250 ml of calcium-fortified soymilk provides around 300 mg calcium. |
Fish | Sardines and canned salmon (bones included) | Half a cup of canned salmon contains 402 mg of calcium. |
Nuts and seeds | Brazil nuts, almonds and sesame seed paste (tahini) | Fifteen almonds contain about 40 mg of calcium. |
Calcium-fortified foods | Breakfast cereals, fruit juices, bread, some plant-based milk | One cup of calcium-fortified breakfast cereal (40 g) contains up to 200 mg of calcium. Half a cup of calcium-fortified orange juice (100 ml) contains up to 80 mg of calcium, and two slices of bread (30 g) provide 200 mg of calcium. Plant-based milk (oat, almond, rice, etc.) may or may not be calcium-fortified, so it is important to check the label of these products if you intend to use these in place of regular dairy milk to boost your calcium intake. |
Box 3: